Vertigo: Getting through the day – one step at a time
Vertigo often gets in the way of our day-to-day activities,1 whether it’s driving to the shops or going out with friends, or even just trying to cook or sleep at home.
Aside from keeping up with your ongoing vertigo treatment,2 there are some other practices that can help prevent the onset of attacks throughout your day.
Sophie*, who has vertigo, has developed a daily routine that works for her. Here are the steps she takes throughout her day to avoid her trigger points.
7 a.m. – Time to wake up
Sophie likes to start her day at 7 a.m. She wakes up feeling refreshed from a good night’s sleep. That’s a great start – sleep is important for the vestibular system, the inner ear’s balance system.3 Vertigo can be a result of disruptions to this balance system.1
Without making any sudden motions,4 Sophie slowly turns on her morning music playlist on her phone and lays still for a while, thinking about the day ahead. When her playlist gets to her favorite song, she gently gets out of bed, careful not to move her head too quickly.1,4 The last time she moved her head suddenly she had a vertigo attack – not something she wants to repeat. Her playlist is calming, and she feels ready for the day ahead.Sophie takes her vertigo medication with a glass of water after breakfast. Her medication gets blood flowing better in the inner ear – this helps with her balance.5 It also normalized the way nerve endings in the inner ear respond to stimuli.5
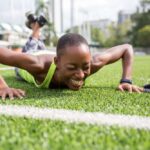
Before heading out, she performs a few vestibular rehabilitation exercises. These are exercises that help to improve the inner ear balance system.1 (See here some simple exercises you can do.)
8:30 a.m. – Commuting to work
Sophie has learnt that certain sights during her commute – such as sitting still on a train but seeing movement through the window – can trigger her vertigo. She finds a forward-facing seat, leans back and closes her eyes.6
This morning, she feels a little bit anxious. It may be the presentation she has to deliver later today, but whatever the reason, she knows it’s not a good sign. Feeling stressed, anxious or tense can trigger vertigo.7,8 She remembers the coping techniques she has learned and takes deep breaths in and out. The train is on its way, and she soon feels better.
Noon – At work
The presentation went brilliantly. But now, back at her desk, Sophie can feel ‘brain fog’ coming on. It’s relatively common in people with vertigo,9 and she’s used to it. In fact, people with vertigo have an eight-fold increased likelihood of having serious difficulty concentrating or remembering, compared to people without vertigo.10 Rather than work through the brain fog, Sophie decides to take an early lunch. She takes her medicine after eating. A stroll around the block in the fresh air does her a lot of good.
6 p.m. – Dinner Sophie’s out for dinner tonight with some of her colleagues. She’s been looking forward to it, but she’s also a bit anxious – the last thing she wants is an attack of vertigo. She knows the types of food she needs to avoid – anything heavy in salt or with the common flavor enhancer called monosodium glutamate, otherwise known as MSG.11,12 She has a glass of wine with the meal as she knows from experience that a moderate amount of alcohol is generally not a trigger for her personally, though it can be for others.12 But she avoids caffeine altogether, as this is a trigger for her, and a common one for people who experience vertigo.12 She has her third dose of medicine for the day with her meal.
10 p.m. – Going to bed
It’s been a good day! A successful day at work, a lovely meal out with colleagues and, best of all, no vertigo. To help her unwind, she does another set of vestibular rehabilitation exercises.1
Now it’s time for bed – Sophie knows about the importance of sleep.3 She also knows that turning over in bed can be a trigger for vertigo,1 so she lies still and relaxes, until she is asleep.
So, that’s Sophie’s routine.
What about your own daily routine? Have you identified your potential triggers? How about writing them down – as a first step to help avoid or overcome them?
* Sophie is a fictional character created for illustrative purposes in this article.